After fifteen months, which felt like forever, from talking to the GP (General Practitioner), completing a 12-month Healthy Weight (HW) programme and finally meeting the NHS (National Health Service) specialist bariatric consultant, I decided to seek private treatment.
The fifteen months leading up to my decision to do that was challenging. When I first decided to go for weight-loss surgery, I felt elated; however, simultaneously, my sister was seriously ill with lung cancer. Then, five months later, my sister died. After that, life did not feel the same. I was, and still am, grief-stricken. When you lose a loved one, it is natural to question and re-evaluate your beliefs and priorities in life. But, although I had already started taking action to pursue bariatric surgery, my sister’s passing strengthened my conviction. I knew I’d made the right decision to get help to optimise my future health.
A parent is not supposed to bury their child, regardless of age. It is not in the correct order of life. My dad passed away years ago, so I wanted to be there for my mum. I live in London in the UK, but I was born and grew up in Stockholm, Sweden, where my mum still lives. One good thing as a result of the pandemic was that many organisations figured out how people can effectively work from home. It meant I could work remotely and be with my mum for a couple of months.
A few days after losing my sister, I encountered another obstacle while preparing to travel to Stockholm. I went to a regular weigh-in as part of the HW programme, where I told them I was going abroad. Apart from the weigh-ins’, I’d had all my therapy-, dietician- and activity coach sessions over the phone. As we were in the middle of the pandemic, the guidance also stated that if you were uncomfortable attending in person, you could weigh yourself at home and report it back to the HW practitioner. So, I hadn’t expected any issues to arise with me going abroad for a period. Instead, they told me I would have to start again when I returned to the UK – I was three months into the programme at that point. They said they wouldn’t treat me while abroad. I was FUMING! It didn’t make any sense. How I managed to keep my composure, I don’t know, but I did. Instead, I asked if they could make an exception since I’d suffered a family loss. They were going to check with a supervisor and come back to me. I left and sat in my car in the clinic’s car park, bawling my eyes out.
After 15 minutes of tears running down my face and an emotional phone call to my mum, I made my way home. As I pulled up outside my house, my mobile phone rang; as promised, the HW practitioner had checked with the supervisor, and everything was fine. I would not need to start again when I returned to London, and the treatment would continue while I was away as it had – over the phone. I could have done without the upset and the stress of it, though.
To receive weight-loss surgery treatment through the NHS in the UK can be difficult and seemingly unnecessarily so. The process patients must go through is agony when they already fit the criteria set by the NHS. Having weight loss surgery is not a quick fix, nor should it be looked upon as some kind of cosmetic vanity surgery. It is a medical procedure that will save lives and ultimately costs by reducing the development of comorbidities. Weight loss surgery will have a significant impact on a person’s life, both physical and emotional. Thus, I would argue that the format of the HW programme would be much more beneficial as a post-surgery resource. Any necessary pre-surgery preparation can be covered solely by the services at the bariatric clinic. It seems redundant that a GP cannot refer a patient directly to a bariatric specialist; since, at that point, the GP should have established that the patient’s previous attempts to lose weight have been unsuccessful.
The list below outlines the criteria for when weight loss surgery is available on the NHS:
- you have a body mass index (BMI) of 40 or more, or a BMI between 35 and 40 and an obesity-related condition that might improve if you lost weight (such as type 2 diabetes or high blood pressure)
- you’ve tried all other weight loss methods, such as dieting and exercise, but have struggled to lose weight or keep it off
- you agree to long-term follow-up after surgery – such as making healthy lifestyle changes and attending regular check-ups
People who might benefit from bariatric surgery don’t know it is a viable treatment option. Many don’t even seek help from their healthcare provider because of the stigma attached to fatness. Instead, they join a weight loss club or start a diet plan based on calorie reduction and exercise to burn more calories. When the diet and exercise plan collapses, people put the ‘failure’ down to poor character. Because this is what society tells us, fat people are lazy, lack discipline and eat nothing but unhealthy foods. Fat phobia is living large in the UK (and across the world).
Another problem, and it is a huge one, is that knowledge about effective obesity treatment is still lacking among health practitioners. They are still harping on with the ‘eat less, move more’ approach, which has proved ineffective for most obese patients. Also, keep in mind that health professionals are not immune to the deep-rooted misconception about fatness and the impossible societal beauty ideals. More importantly, they are not necessarily well-educated in the complex factors causing obesity, such as abnormal regulation of energy balance (which is influenced by genetics, hormones, etc.). Energy balance is not as simple as the balance between calories consumed and energy expenditure (basal metabolic rate(*) + physical activity), which is the driving concept of ‘eat less, move more’.
When excessive weight is sustained over an extended period, the chances of shaking it off and maintaining weight loss with diet and exercise become slimmer (excuse the pun). The ‘set point’ theory explains how your body fights to maintain the elevated weight, making it nearly impossible to sustain a significant weight loss achieved by a calorie-controlled diet. Yet, surprisingly, the set point theory is not public knowledge or widely known within the health profession (or industry) outside of metabolic/bariatric specialists.
Your body is very clever, but it has not adapted to the relatively recent increase in food availability over the last 40-50 years; its instinct is survival. Throughout human history, the body has negotiated survival in a state of starvation (for thousands of years) more than in an environment of abundant food availability. Hence, it’s not surprising the body is protecting the excess – it’s conditioned to build a reservoir in case of future scarcity. Also, the body doesn’t care what it looks like.
Despite the 30 minutes of upset where I thought I would have to restart the 12-month HW programme, I persevered. Just a couple of days before I travelled to Sweden, I met with the regional specialist consultant assigned to the HW programme to provide guidance and assess your suitability for surgery. Taking my knowledge and experience into account, I found that talking to a bariatric consultant was probably the most helpful element of the 12-month programme. Fast forward ten months, when I had completed the HW programme, I sat in the same consultant’s clinic in a South London Hospital on a beautiful August morning. That’s when I received the gut-wrenching news that the current waiting time for surgery was 3 to 5 years.
That afternoon, I called a well-renowned clinic in Stockholm, which referred me to GB Obesitas in the south of Sweden. This was when I experienced a fundamental shift, and things started moving at my preferred pace (‘make it happen now’). The most amazing nurse called me in response to a brief email explaining my circumstances. I had comprehensive information sent to me backing up what the nurse had outlined to me over the phone. It can be overwhelming to receive a lot of information in one go, so the guidance notes were beneficial as I could revisit the guidance when needed. Finally, we booked a date for surgery in November 2022.
The ball really got started rolling from there on. I attended an online information group meeting, a 1:1 consultation with the bariatric consultant, did blood tests through my GP surgery in London, emailed the results to the clinic nurse, and then started the pre-op diet. I will tell you more about the pre-op diet in a separate post.
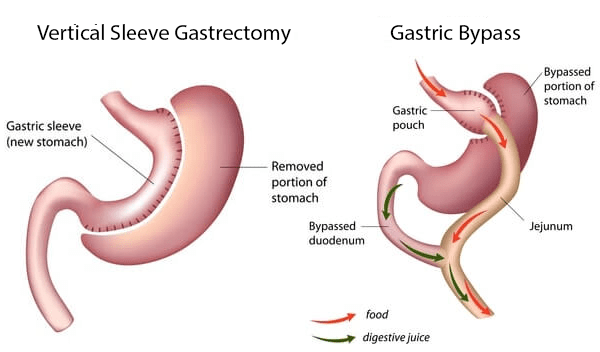
I was excited that I finally had a date for surgery. From the beginning, I had been pretty set on having gastric sleeve surgery, which I had discussed with the consultant in London. However, after talking to the consultant in Sweden, I changed my mind. By their recommendation, I decided to have a gastric bypass instead. Both surgeries are very effective, but the bypass generally generates more significant weight loss, approximately 80% of the excess weight compared to 70% with a sleeve. Thus, the bypass is generally a better option for someone like me with a very high BMI and you have more weight to lose. Ultimately, that was the deciding factor for me to choose gastric bypass surgery over a gastric sleeve.
If you are considering bariatric surgery, do your due diligence and research which surgery might suit your circumstances best. For example, if you already have acid reflux problems, it can get worse after gastric sleeve surgery, and it is also something that might start to occur even if you haven’t suffered from it before. Also, smoking can cause ulcers after bariatric surgery – especially with a gastric sleeve. Finally, among the side effects of gastric bypass is bowel obstruction which would require another surgery.
All this is due to the difference in post-surgery anatomy and not the surgeon’s skill level. Discuss your preference with your consultant but be receptive to their professional recommendation. After all, you want to achieve the best possible long-term health outcomes.
You might find the YouTube video below helpful in your research, where the American doctor John Pilcher explains how the two different surgeries work and the difference between the two (gastric sleeve and gastric bypass).
I wish you great success and all the best if you are about to set off on a journey exploring bariatric surgery.
All is well.
Milla ♥
(*) basal metabolic rate – the amount of energy expended while at complete rest